Melasma is a skin condition that causes discolored patches and freckle-like spots on the face. They usually appear on the cheeks, chin, forehead, nose bridge, upper lips, and neck. Although they do not cause any harm or be a sign of any medical emergency, they can still largely affect one’s confidence, especially today when having clear skin is the trend and everyone is heavily invested in their skin care routines.
Melasma’s effect on someone goes beyond the skin. People with melasma have been shown to have a diminished quality of life since the condition influences their social interactions and their mental and emotional well-being.
Causes of Melasma
Melasma can affect anyone, but the risk is higher for women, especially those who are pregnant, taking contraceptive pills, and exposed to intense sunlight. Other factors that can cause melasma are wide-ranging, from genetics to lifestyle and environmental stress. Having a good understanding of these factors can help in choosing proper treatment regimens and preventive measures to take.
Genetics
Genetic predisposition is one of the main factors that contributes to the development of melasma. Gender and heredity play a major role with women, and people with family members who had melasma are more prone to having the condition.
Hormones
Fluctuations in hormone levels have been shown to contribute to melasma development. During the third trimester of pregnancy, there is normally an increase in the levels of estrogen, progesterone, and melanocyte-stimulating hormone (MSH). Although the exact mechanism is unknown, this increase in these hormones is a factor in melasma development.
Similarly, menopausal women who are taking progesterone have been shown to have higher risks of developing melasma than those taking estrogen alone. This implicates progesterone as a factor in melasma.
Similarly, those who are on medications such as contraceptive pills (both estrogen- and progesterone-containing) and diethylstilbestrol in men with prostate cancer are observed to develop melasma.
Sunlight & UV Radiation
Exposure to intense sunlight can cause UV damage to cells, causing lipid peroxidation that results in free radicals that can stimulate melanocytes to produce excess melanin. Blue light or visible radiation exposure is also found to stimulate Opsin-3 receptors that directly affect melanin production.
Lifestyle & Stress
Oxidative stress is also shown to have a direct effect on melasma development. Similarly, using harsh chemicals such as peeling agents and bleaching agents that cause thinning of the skin and make it more susceptible to damage can also contribute to melasma development.
When to See a Dermatologist
Self-diagnosis is never advisable when it comes to skin conditions such as melasma. Tests such as the Wood’s Lamp test can help determine which layers of the skin are affected. Moreover, a consultation with a dermatologist can help you choose the right treatment options that are available to you.
Does Melasma Go Away on Its Own?
Yes, melasma can go away on its own. However, this depends on the cause. Melasma that develops during pregnancy and those that are caused by certain medications typically go away after giving birth or after stopping the medication. It is also important to note that you should never self-medicate or try out treatment options for melasma during pregnancy without consulting an expert first. This is because some of the agents used to treat melasma can cause severe harm to the fetus.
Treatment Options
Unfortunately, for most people, melasma doesn’t resolve on its own and requires intervention. Treatment options range from topical creams and solutions to chemical peels, lasers, and oral medications.
Topical Treatment
Topical treatments such as hydroquinone, tretinoin, and fluocinolone acetonide are considered the first-line agents for melasma. They can be used in triple combination, dual combination, or as single agents, especially when hypersensitivity to certain agents develops. Hydroquinone and tretinoin are known to be contraindicated in pregnant and breastfeeding women as they can cause a range of complications.
Additionally, agents like tranexamic acid and azelaic acid are also used to speed up the skin’s cell turnover rate, causing newer skin to come to the surface faster. These agents can be highly effective but can also cause devastating adverse effects when used incorrectly; thus, it is very important to consult your dermatologist prior to using any of them.
Oral Medications
Options in this category are often food supplements with antioxidant effects, with the exception of tranexamic acid and procyanidin. Antioxidants such as vitamins C and E and carotenoids are known to combat the effects of oxidative stress and free radicals.
The use of tranexamic acid for melasma, on the other hand, is considered an "off-label use." This means that the drug is meant for other conditions but has been shown to have an effect on melasma. Tranexamic acid is prescribed for bleeding disorders, so its use should be under the supervision of a physician as it can cause adverse effects such as deep vein thrombosis.
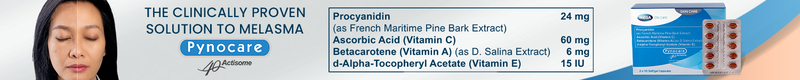
Lastly, procyanidin is the active ingredient of Pynocare, the only FDA-approved medication for melasma that is available in the Philippines. In addition to procyanidin, Pynocare also contains antioxidants such as vitamins A, C, and E that work together to target the cellular mechanisms that contribute to the development of melasma.
Pynocare has been clinically proven to reduce the appearance of melasma when taken twice a day for 8 to 12 weeks. It has also been shown to have very few or no side effects at all.
Chemical Peels & Lasers
Peels and lasers are also being used in melasma treatment; however, they carry the risk of severe adverse effects and are reserved as a last resort.
Preventing Melasma
Avoiding sun exposure is the cornerstone of preventing melasma. The use of sunscreens or sunblocks is also highly encouraged. Use sunscreen/sunblock that blocks both UVB and UVA rays since most formulations only block UVB rays, and UVA and visible radiation (between 320 and 700 nm in the spectrum) have been shown to stimulate melanin production.
Pynocare can also be taken as a preventive measure when taken once a day, especially for those who are at a higher risk of developing melasma.
References
-
Basit, H., Godse, K. V., & Al Aboud, A. M. (2022). Melasma. In StatPearls. StatPearls Publishing.
-
Handog, E.B., Galang, D.A.V.F., De Leon-Godinez, M.A., & Chan, G.P. (2009). A randomized, double-blind, placebo-controlled trial of oral procyanidin with vitamins A, C, E for melasma among Filipino women. International Journal of Dermatology, (48), pp. 896-901. https://doi.org/10.1111/j.1365-4632.2009.04130.x
-
Silpa-archa, N., Kohli, I., Chaowattanapanit, S., Lim, H.W., & Hamzavi, I. (2017). Postinflammatory hyperpigmentation: A comprehensive overview: Epidemiology, pathogenesis, clinical presentation, and noninvasive assessment technique. Journal of the American Academy of Dermatology, 77(4), pp. 591-605. https://doi.org/10.1016/j.jaad.2017.01.035