The cause of melasma is interplay of various factors from genetics to certain medications. This makes it hard for most people who are experiencing this condition to find a treatment that is effective and reliable. It has been known for some time that melasma begins when the cells that give the skin its color (melanocytes) accelerate and go into overdrive. Although the exact reason for this is not yet fully understood, there are topical treatments that can be used and ways on how to cure melasma from the inside.
Melasma is a common skin disorder that appears as dark spots on the skin. The color can appear as light brown spots or blue-grayish patches on the skin. These dark skin spots are mostly found on the face, cheeks, and forehead. Dark patches may gradually occur on the shoulders and forearms too. Although melasma is essentially harmless, if progressive and persistent, it can dampen a person’s self-confidence and might affect their overall mental health.
Triggers of melasma
It is possible that melasma develops when the normal physiologic processes of skin cells are disrupted. Some possible risk factors include:
Pregnancy: studies have shown that women are more susceptible to melasma, especially pregnant women. The increased levels of estrogen, progesterone, and melanocyte-stimulating hormone in pregnant women are thought to trigger and cause melasma. Melasma that occurs during pregnancy is expected to fade afterward, but in some cases, the melasma persists even after giving birth.
Overexposure to sunlight: melanin is produced more once the skin is hit by sunlight. This is due to UV radiation causing lipid peroxidation that damages cell membranes and results in free radicals stimulating melanin production. So, exposing the skin to too much sunlight may cause melasma to trigger or flare up.
Phototoxic drugs: some drugs can cause a reaction on the skin called a phototoxic reaction where the skin becomes more sensitive to sunlight. It is said that around 10 to 20% of hyperpigmentation cases are attributed to phototoxic drugs. These include some antibiotics, nonsteroidal anti-inflammatory drugs (NSAIDS), diuretics, retinoids, hypoglycemics, antipsychotics, etc. These drugs should not be avoided entirely but you need to take precautions when prescribed with them.
Other medications: contraceptives and anti-seizure medications are also believed to trigger melasma in some people.
Tanning beds: in addition to sunlight and UV rays, tanning beds also produce the same effects on the skin.
Stress: some researchers suggest that stress may contribute to the development of melasma, as stress causes increased production of cortisol, which may trigger reactions that can lead to melasma.
Genetics: genetic predisposition is said to be a major factor in melasma development. Researchers suggest that it is hereditary since approximately 33% to 50% of patients experiencing melasma have disclosed that it is also experienced by other family members.
Treating melasma from the inside
Since melasma can be caused by many different factors, treating it can be quite a challenge. Treatment may also vary from one patient to another. An approach commonly used by dermatologists is to address the factors linked to melasma. This is a strategy that medical practitioners carry out how to cure melasma from the inside. Some of the available treatments today are outlined below.
Balancing hormones: an ideal strategy to treat melasma is to address the linked trigger, a doctor may advise a patient to treat melasma after birth if the trigger is pregnancy or changing their current oral contraceptives to another one. Melasma linked to oral contraceptives usually fades after discontinuing specific medications.
Diet: there is no proven dietary treatment for melasma, however, maintaining healthy skin may control the effects of melasma. Adequate amounts of fluid and adding foods that are rich in vitamin D, such as almond milk, eggs, meat, fish, yogurt, etc. can improve the overall appearance of the skin. Vitamin C rich foods can also help in controlling excessive production of melanin and providing photoprotection from the harmful rays of the sun.
Reduce stress: cortisol levels are increased when we are stressed, and it may have a role in contributing to the development of melasma. Understanding the causes of stress and knowing how to manage them properly can help in avoiding the development of melasma.
Other treatments: Treatments that are a combination of therapies are also beneficial. Some of these treatments include sunscreen for sun protection, hydroquinone, which is a common skin whitening ingredient to decrease melanocytes, tretinoin and a mild corticosteroid, or a combination of the three.
There are also treatments for melasma that can help with faster results. Most of these procedures require a doctor’s appointment and are external procedures. These procedures include:
Chemical peel: a procedure that uses a chemical solution to remove the outer layer of the skin, promoting fresher and rejuvenated skin. An example of a chemical peel is a salicylic acid peel.
Microneedling: also known as collagen induction therapy, this treatment uses a roller with tiny needles that penetrate the skin deeply to stimulate collagen and elastin production. Research suggests that this procedure, combined with skin lightening creams containing topical retinoid, vitamin C serums, or hydroquinone creams, is more effective in fading dark spots caused by melasma.
LED Light therapy: this procedure uses light therapy to improve the cell function of the skin. There are different types of LED light therapy, and it is based on the wavelengths of the therapy at which a skin disorder is targeted. Specifically, green light therapy is helpful in fading hyperpigmentation on the skin, since the wavelengths that it produces help decrease the production of melanin.
Oral medication: One oral medication usually prescribed by dermatologists is tranexamic acid that is taken twice daily. In a recent study, it is found that oral tranexamic acid demonstrated the efficacy for melasma, especially in Asians. Even in low doses, tranexamic acid exhibited positive results in a span of 8 to 12 weeks.
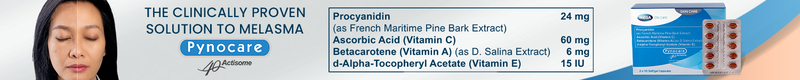
Another oral solution for melasma is Pynocare. It is a clinically proven formulation to help reduce the appearance of melasma. It is the only FDA–approved oral treatment for melasma, so it is a safe option to choose from on how to cure melasma from the inside. Research shows that with continuous use of Pynocare, the dark spots caused by melasma are reduced within 8 weeks. Pynocare is formulated with specific ingredients that work synergistically with each other to reduce the appearance of melasma and disrupt some of the pathways that cause it.
-
Beta-carotene: also known as vitamin A, this ingredient supports nourishment from deep within the skin to reduce the appearance, and to fade dark spots easily.
-
Ascorbic acid: more commonly known as vitamin C, it has been proven to help provide cellular protection against damage and is also commonly used as a treatment for other forms of hyperpigmentation.
-
d-alpha-tocopheryl acetate: this ingredient is a powerful antioxidant that also provides protection from UV rays, decreasing sun damage on the skin.
-
Procyanidin: this ingredient has antioxidant and anti-inflammatory properties that are good options in treating melasma from the inside. Procyanidin, combined with vitamins A, C, and E is proven safe and effective in treating dark spots caused by melasma.
Even though melasma does not cause any harm to the body, it can still have adverse effects on the emotional and mental health of an individual suffering from it. This is a natural response to whatever flaws the physical appearance, especially in today’s society where outside appearance affects how people treat others. Knowing the proper way to deal with melasma by consulting a dermatologist is one way to go about it, but learning how to take care of yourself will certainly be of great help.
References
-
Trivedi, M. K., Yang, F. C., & Cho, B. K. (2017). A review of laser and light therapy in melasma.
-
International journal of women's dermatology, 3(1), 11–20. https://doi.org/10.1016/j.ijwd.2017.01.004
-
Handog, E. B., Galang, D. A., de Leon-Godinez, M. A., & Chan, G. P. (2009). A randomized, double-blind, placebo-controlled trial of oral procyanidin with vitamins A, C, E for melasma among Filipino women. International journal of dermatology, 48(8), 896–901. https://doi.org/10.1111/j.1365-4632.2009.04130.x
-
Ludmann, P. (2022). Melasma: Causes. From https://www.aad.org/public/diseases/a-z/melasma-causes
-
Paul, R. (2021). Finally, a More Effective Treatment for Melasma. From https://www.centerfordermatologyandlaserskinsurgery.com/skin-care/finally-a-more-effective-treatmen t-for-melasma
-
Bailey, A. (2022). LED Light Therapy for Skin: A Complete Guide. From https://www.verywellhealth.com/led-light-therapy-5217765
-
Giorgi, A. (2022). How to Cure Melasma From the Inside. From https://www.verywellhealth.com/how-to-cure-melasma-from-the-inside-5272264
-
Splane, B. (2022). Types of Cosmetic Laser Procedures. From https://www.verywellhealth.com/cosmetic-laser-procedures-decoding-2710211
-
Cleveland Clinic. (2020). Melasma. From https://my.clevelandclinic.org/health/diseases/21454-melasma
Article Reviewed by: Dra. Carol Carpio