Melasma, colloquially known as pekas among Filipinos, is a common skin condition that presents as brown to blue-gray patches on the skin, usually on the nose, forehead, cheeks, and upper lip. Melasma is painless and harmless, albeit considered as a source of distress by many due to the uneven skin tone it causes. Melasma can be treated with help from a trusted dermatologist and accurate knowledge on how to remove pekas on face.
What causes melasma?
Melasma is caused by a variety of factors, one of which is exposure to ultraviolet radiation such as that emitted by the sun and tanning beds. Another factor is genetics: around 50% of people with melasma report having family members with the same condition. Melasma is also more commonly found in women of reproductive age, with around 90% of cases affecting women. People with darker skin tones are also more likely to develop melasma. Hormones have also been linked to pekas. Increased progesterone and estrogen levels are associated with melasma, which is why it is often found in pregnant women as well as those taking birth control pills or other medications that cause spikes in hormones. Finally, thyroid disease has also been identified as a factor, with research showing a link between hyperthyroidism and hyperpigmentation.
Ways to remove pekas on face
While many women have pekas, it is not necessarily a permanent skin condition. Here are some answers to the question how to remove pekas on face.
#1: Protection from the sun
As mentioned, one of the main causes of melasma is exposure to UV radiation. Avoiding sun exposure is therefore a crucial part of treating this condition. Bear in mind that this doesn’t mean simply steering clear of direct sunlight. Exposure to visible light such as that streaming through windows can contribute to pekas, which is why dermatologists also recommend wearing broad-spectrum tinted sunscreens, as this offers protection against UV radiation. And don’t forget that avoiding UV radiation includes shunning tanning beds, since these emit UV rays as well.
#2: Identification of triggers and contributing factors
Identifying triggers and contributing factors is also part of removing pekas. There are instances when melasma resolves on its own. For instance, melasma caused by pregnancy usually fades after a few months. Melasma caused by contraceptive pills or other medications also often goes away once a person stops taking them. Moreover, some substances aggravate pekas by causing inflammation that results in hyperpigmentation. These may include harsh soaps, cleansers, and cosmetics. Even stress has been linked to this condition by some studies. It is therefore important to consider identifying the cause of pekas in the course of treatment, as simply avoiding it may be enough to address the condition.
#3: Oral supplements
Taking oral supplements is another way to treat melasma. There are various supplements available on the market. Antioxidants, for instance, are widely used as a treatment for melasma due to the link between melasma and oxidative stress, which results from an imbalance in free radicals and antioxidants in the body. Antioxidants such as glutathione and vitamin C are usually included in treatment regimens, given the promising evidence of their therapeutic effect on melasma.
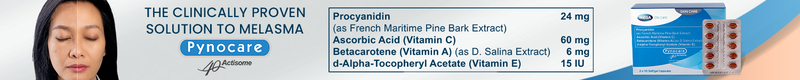
Another effective oral supplement is Pynocare, which contains procyanidin and antioxidant vitamins A, C, and E. As an oral supplement, Pynocare treats melasma by normalizing melanin levels deep in the inner layers of the skin. One study conducted among Filipino women with melasma showed that taking Pynocare yields positive results in as short as eight weeks.
#4: Topical treatments
Removing melasma also commonly involves the prescription of topical treatments. These are creams or gels applied directly on the skin. One of the most commonly used topical treatments is hydroquinone or HQ, which acts by inhibiting the production of melanin by the skin. HQ also frequently comes in triple combination (TC) form, which is when it is combined with retinoids such as tretinoin and corticosteroids such as mometasone furoate or fluocinolone acetonide to optimize the efficacy of treatment. Studies show that hydroquinone and TC can be used for up to six months, although HQ and tretinoin should not be used during pregnancy.
Other examples of topical treatments include niacinamide and azelaic acid, both of which are considered safe for use by pregnant and breastfeeding women. There is also some evidence that vitamin C, kojic acid, and melatonin can aid in the removal of pekas.
#5: Chemical peeling
Apart from oral supplements and topical treatments, melasma is also often removed through chemical peeling. The process involves the controlled application of substances that cause the removal of the skin’s superficial layer, thus eliminating excess melanin. Some of the most commonly used agents for chemical peeling are glycolic acid, salicylic acid, and tretinoin. Note that chemical peeling is not the first line of treatment but instead is often done in conjunction with topical agents. Moreover, chemical peeling is applicable to melasma found in the epidermis or upper layer of the skin, but not to dermal melasma, since this type of pekas is located in the deeper layer.
#6: Laser treatments
Laser treatments have also been used to remove pekas. Some studies show that various laser treatments yield positive results. These should be used with care, however. One review of various laser treatments, for instance, recommends resorting to these therapies only when first-line and second-line treatments such as topical depigmenting agents and chemical peels have failed.
#7: Microneedling
Microneedling is another method shown to have a positive effect on melasma. This minimally invasive procedure involves driving thin needles into the upper layer of the skin, thus causing minute tears. Originally indicated for the treatment of scars, microneedling is now also used to remove pekas, as the hyperpigmentation tends to decrease once the skin heals from the tears.
Getting the right treatment
The emotional and psychosocial distress caused by pekas is both widely known and well-documented. It is not uncommon for people to feel embarrassed, depressed, or frustrated by this condition. Fortunately, the wide range of available treatments offers hope. When seeking treatment, it is best to consult with a trusted dermatologist who knows how to remove pekas on face, especially since removing pekas is not simply a matter of choosing one therapy. Oftentimes, treating melasma involves a combination of two or more ways in order to optimize efficacy. Working closely with your dermatologist will help uncover the specifics of your case and formulate an approach that best fits your needs and preferences.
References
-
Arora, P., Sarkar, R., Garg, V. K., & Arya, L. (2012). Lasers for treatment of melasma and post-inflammatory hyperpigmentation. Journal of Cutaneous and Aesthetic Surgery, 5(2), 93–103. https://doi.org/10.4103/0974-2077.99436
-
Babbush, K. M., Babbush, R. A., & Khachemoune, A. (2020). The therapeutic use of antioxidants for melasma. Journal of Drugs in Dermatology, 19(8), 788–792. https://doi.org/10.36849/JDD.2020.5079
-
Basit, H., Godse, K. V., & Al Aboud, A. M. (2023, April 16). Melasma. In StatPearls. StatPearls Publishing. Retrieved July 18, 2023, from https://www.ncbi.nlm.nih.gov/books/NBK459271/
-
Çakmak, S. K., Özcan, N., Kılıç, A., Koparal, S., Artüz, F., Çakmak, A., & Köse, K. (2015). Etiopathogenetic factors, thyroid functions and thyroid autoimmunity in melasma patients. Postepy Dermatologii i Alergologii, 32(5), 327–330. https://doi.org/10.5114/pdia.2015.54742
-
Cassiano, D. P., Espósito, A. C. C., da Silva, C. N., Lima, P. B., Dias, J. A. F., Hassun, K., Miot, L. D. B., Miot, H. A., & Bagatin, E. (2022). Update on melasma-part II: Treatment. Dermatology and Therapy, 12(9), 1989–2012. https://doi.org/10.1007/s13555-022-00780-4
-
Cleveland Clinic. (2020, July 27). Melasma. Retrieved July 18, 2023, from https://my.clevelandclinic.org/health/diseases/21454-melasma
-
Correia, G., & Magina, S. (2023). Efficacy of topical vitamin C in melasma and photoaging: A systematic review. Journal of Cosmetic Dermatology, 22(7), 1938–1945. https://doi.org/10.1111/jocd.15748
-
Garibyan, L. (2022, July 11). Melasma: What are the best treatments? Harvard Health Publishing. Retrieved July 18, 2023, from https://www.health.harvard.edu/blog/melasma-what-are-the-best-treatments-202207112776
-
Godse K. V. (2009). Triple combination of hydroquinone, tretinoin and mometasone furoate with glycolic acid peels in melasma. Indian Journal of Dermatology, 54(1), 92–93. https://doi.org/10.4103/0019-5154.49005
-
Handel, A. C., Miot, L. D., & Miot, H. A. (2014). Melasma: a clinical and epidemiological review. Anais Brasileiros de Dermatologia, 89(5), 771–782. https://doi.org/10.1590/abd1806-4841.20143063
-
Handog, E. B., Galang, D. A., de Leon-Godinez, M. A., & Chan, G. P. (2009). A randomized, double-blind, placebo-controlled trial of oral procyanidin with vitamins A, C, E for melasma among Filipino women. International Journal of Dermatology, 48(8), 896–901. https://doi.org/10.1111/j.1365-4632.2009.04130.x
-
Katiyar, S., & Yadav, D. (2022). Correlation of oxidative stress with melasma: An overview. Current Pharmaceutical Design, 28(3), 225–231. https://doi.org/10.2174/1381612827666211104154928
-
Ludmann, P. (2022, February 15). Melasma: Causes. American Academy of Dermatology. Retrieved July 18, 2023, from https://www.aad.org/public/diseases/a-z/melasma-causes
-
Sarkar, R., Arsiwala, S., Dubey, N., Sonthalia, S., Das, A., Arya, L., Gokhale, N., Torsekar, R. G., Somani, V. K., Majid, I., Godse, K., Ravichandran, G., Singh, M., Aurangabadkar, S., Salim, T., Shah, S., & Sinha, S. (2017). Chemical peels in melasma: A review with consensus recommendations by Indian pigmentary expert group. Indian Journal of Dermatology, 62(6), 578–584. https://doi.org/10.4103/ijd.IJD_490_17
-
Sarkar, R., Bansal, S., & Garg, V. K. (2012). Chemical peels for melasma in dark-skinned patients. Journal of Cutaneous and Aesthetic Surgery, 5(4), 247–253. https://doi.org/10.4103/0974-2077.104912
Article Reviewed by: Dra. Carol Carpio